The problem with obesity
This blog has been written by Dr Barry Lambert, consultant paediatric anaesthetist caring for babies and children undergoing surgery at Birmingham Childrens’ Hospital and co-founder of Medstars.
Obesity is a significant risk when undergoing surgery – fact. As medics we know this. Apart from the practical issues of managing a patient’s positioning on an operating table, there are increased technical challenges to placing intravenous drips and managing the airway safely. Reaching the part of the body requiring surgery is more difficult and the surgical equipment has to be longer. All this and more and that’s even before you consider the impact of medical conditions associated with obesity affecting surgical risk such as high blood pressure and diabetes.
So why do we have such problems clearly communicating the issue of weight with our patients?

Since it is now good practice to copy our patients into the letters we write about them, we are even opaque when referring patients between fellow professional medics. Obesity is a taboo word. The disapproval of this outlawed medical condition easily infects other medical terms such as BMI (body mass index. BMI = a person’s weight in kilograms divided by their height in metres squared). To consider speaking plainly and jargon free to suggest to your patient a discussion about their weight or even mention that they are overweight makes us squirm. Saying the word fat is obviously verboten!
This was clearly highlighted by a recent patient referral letter asking me to assess the suitability of a patient for surgery. The central issue was obesity. This was referred to by only a note suggesting a “high plot on the patient’s growth chart”. Unsurprisingly the patient was taken aback to discover that they were in clinic because of their weight.
Our medical angst is an extension of our society’s problem with weight. Cancer Research UK’s obesity campaign highlighting the fact that obesity is the second most preventable cause of cancer, resulted in a backlash of complaints from social media and the press accusing the charity of body or fat shaming.
WW or previously Weight Watchers has ditched any reference to Weight. The company’s new strap line is “wellness that works”. Mindy Grossman the new CEO of WW described the firm as shifting from a focus on just weight loss to its broader remit looking at “wellness”. She went on to say to the BBC “The paradox is that everyone is talking about wellness and nobody wants to use [the words] diet or weight, but we’re not getting healthier,” Ms Grossman said. The rebrand is designed to attract more potential users, but also to encourage their 2.7M subscribers to stay with them long-term as most WWs never reach their desired W.
Understanding the size and potential significance of the problem in society is sobering. 40% of men are overweight and 26% are considered obese (a BMI of 30 or greater). Whilst 30% of women are overweight and 27% are obese.
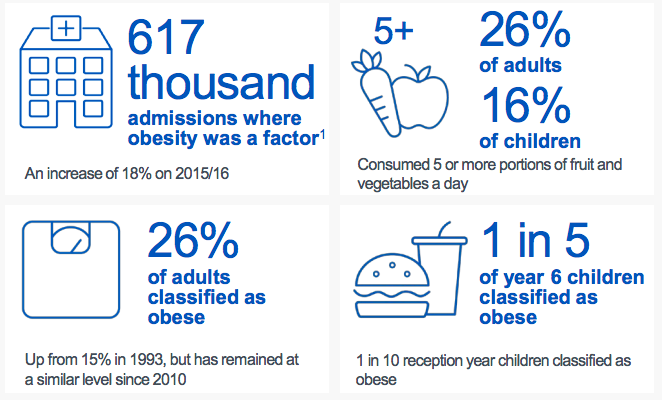
One fifth of our future generation are already obese by the age of 10 years. The strain on our health can be seen in the rising rates of NHS hospital admissions where obesity was considered a factor.
We need to recognise and change the structural problems with the way we live and work that are making it so easy to be overweight. As the problem with obesity gets greater so does our inability to discuss it. We need to break the taboos and society’s censure. The more we recognise problems with weight and learn to use language that is acceptable to all only then can we help ourselves, help our patients and truly watch our weight.
If you’ve tried and failed to lose weight, a visit to a GP could help.
Dietitian, Ms Claire Fudge, has expertise in weight management and specialist diets for medical conditions such as diabetes.
Medstars Medical Concierge Service
Looking for extra guidance when it comes to your healthcare? Sometimes interpreting medical information and making the best decisions can be daunting and complicated. Our private medical concierge service provides easy access to top UK health experts. We guide our patients with genuine choice and trust, offering a bespoke service for anyone in the world seeking private UK healthcare. Learn more about Medstars Medical Concierge Service. Want to learn more about providing our medical concierge service as an employee benefit? Learn more about Medstars Medical Concierge for Business.

